All Nonfiction
- Bullying
- Books
- Academic
- Author Interviews
- Celebrity interviews
- College Articles
- College Essays
- Educator of the Year
- Heroes
- Interviews
- Memoir
- Personal Experience
- Sports
- Travel & Culture
All Opinions
- Bullying
- Current Events / Politics
- Discrimination
- Drugs / Alcohol / Smoking
- Entertainment / Celebrities
- Environment
- Love / Relationships
- Movies / Music / TV
- Pop Culture / Trends
- School / College
- Social Issues / Civics
- Spirituality / Religion
- Sports / Hobbies
All Hot Topics
- Bullying
- Community Service
- Environment
- Health
- Letters to the Editor
- Pride & Prejudice
- What Matters
- Back
Summer Guide
- Program Links
- Program Reviews
- Back
College Guide
- College Links
- College Reviews
- College Essays
- College Articles
- Back
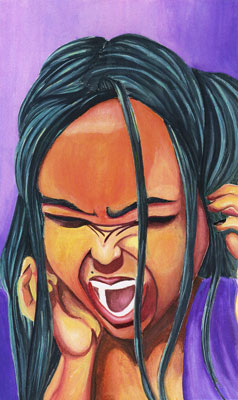
Making Connections: Intersectionality in Mental Health Treatment and Diagno
Last spring, students at Ithaca College held a panel to raise awareness for mental health. The students discussed their personal experiences with mental illness in marginalized communities, and opened a conversation in an attempt to break the stigma. In 1989, Kimberle Crenshaw coined the term “intersectionality” to refer to the different identities that exist within each individual person and how each of those specific identities connect and carry a different weight. One’s unique identity determines how he experiences and perceives life. A black woman faces discrimination for being both black and a woman, but also she is discriminated against for a being a black woman. This is an example of how intersectionality is overlooked as research often separates gender and race without considering the struggles of the two as one. Intersectionality highlights the social factors that affect human lives and the differing groups. The social identities that people are comprised of are significant to one’s mental health. Mental illness is defined as a chemical imbalance of the brain that affects a person’s thinking and mood. Illnesses such as depression, anxiety, autism, etc. hold a great deal of influence in a person’s life and must be treated accordingly and taken into consideration when making even the smallest of choices. Great disparities in mental health lie within racial and ethnic backgrounds. Thirty percent of the world population suffers from mental illness, but only one- third of those affected get the treatment they need (Ngui). Factors such as cultural stigma and discrimination impact whether or not a person is properly diagnosed and receiving the effective treatment. Common methods of treatment neglect to look at the intersectionalities of one’s identity. The implementation of intersectionality in the diagnosis and treatment of mental illness is imperative in the progression and effectiveness of recovery.
Society is divided among several groups such as race, gender, and religion, which serve to define individuals. It is important to understand that each of these groups affect how one perceives and is perceived by the rest of the world. Social identities intersect and affect mental health. The notion of intersectionality is widely overlooked in research for a few reasons. First, there is a lot of power in the world, and it is difficult to convince people to change how they view the entire world. Intersectionality is a complex concept that is often misunderstood by many, with this come several misconceptions. “Racial and gender matters are not mutually exclusive. Identity politics tend to ignore intra-group differences, therefore contributing to tensions among the different groups. The experiences of women of color, specifically black women, are often underrepresented in either feminism or anti-racism.” (Crenshaw) The experiences of women within one culture or race differ from the experiences of women within others. Many of the experiences that black women face are not classified within the traditional boundaries of race and gender discrimination. Ignoring the different experiences prevents an accurate representation of the effects of mental illness.
Great disparities in mental health lie within racial and ethnic background. For many years, African Americans have tended have to higher rates of death, disease and disability than whites. Black people usually have higher levels of psychological distress and lower levels of well-being (Snowden). Stressful life experiences that are linked to race, (poverty, violence, racism, etc.) can also adversely impact the health of minority populations. Psychiatric and behavioral problems among minority youth often result in school punishment or incarceration, but rarely mental health care. “Black and Latino children made, respectively, 37% and 49% fewer visits to psychiatrists and 47% and 58% fewer visits to any mental health professional” (Marrast). The adverse effects of this often lead to a decline in mental condition. Experiences of mental illness and distress taking place in social, historical, and cultural contexts have led to the pathologizing of some groups of people.
One’s experiences of mental distress may occur with an emphasis on the contributions of social and structural factors. Disparities can be accounted to the mistrust of psychiatric doctors and fear of stigma. It is found that practitioners and mental health program administrators make judgments about people on the basis of race or ethnicity. Biased views can be held knowingly or unknowingly but can result in action or a failure to act. “African, Asian, Native, and Latino Americans needing outpatient care are unlikely to receive it. bias partially explains disparities” (Snowden). There is great distrust of the systems and institutions for reason, and a long legacy of distrust of people in the health profession. In order to reach out to communities it is important to gain their trust. People need to feel understood in order to understand their mental health and be willing to heal.
Culture is an important factor when treating mental illness because it determines how an illness is defined, how, and where help is sought. While stigma of mental illness is prominent in society, it is especially apparent in ethnic and racial cultures. Intersectionality can help to combat certain stigmas against mental illness. Stigma itself is a social construct, heavily influenced by socially important categories such as culture. “Collectivist aspects of some Asian groups, for example, may lead to perceptions that disabilities of mental illness reflect flaws of the family” (Corrigan). Someone who is experiencing symptoms of mental illness may not express this as he/she would be afraid to bring shame to their family. In addition to this, the idea of mental illness is foreign to some groups. Some communities do not have the proper resources to educate the people on mental health and treat it. Those suffering with mental illness in developing countries may also be burdened with stigma and discrimination. Mental disorders account for an enormous global burden of disease that is largely underestimated and underappreciated (Ngui). The lack of proper resources can lead to misconceptions about mental illness.
The use of intersectionality in treatment and diagnosis is necessary in order to improve the conditions of those suffering. In health research, intersectionality provides a more precise identification of inequalities (Bauer). This ensures that strategies are relevant to specific cultures. The inclusion of culture and cultural factors in psychiatric diagnosis would benefit the system as a whole. Physician Renato D. Alarcorn states, “The cultural content of psychiatric diagnosis should include the main, well-recognized cultural variables, adequate family data, explanatory models, and strengths and weaknesses of every individual patient”. The use of culture in current psychiatric diagnostic practice is very poorly addressed, although the patient’s cultural background and identity must be thoroughly understood by the clinician, and its impact recognized and evaluated.
Intersectionality requires that someone’s entire existence as a whole is considered rather than breaking them down to different aspects. It is important to listen not only to the patient, but also to their carers and community to enable the clinician to provide more efficient help (Bhugra). A few cautions must be taken when treating a patient. There is a misconception to think of intersectionality as one’s individual identity. Intersectionality has to include an attention to systems, policies, and prophecies.
Intersectionality is often confused with cultural competency. While quite similar, there is a difference between the two. An intersectional approach is different from a culturally competent one in two ways. The first is the most commonly known. Instead of just focusing on one aspect of identity, the focus is on multiple categories. It looks at someone as their race/gender/class all together. Individuals who are members of multiply marginalised groups cannot simply dissect out the “types” of oppression specific to each part of their identity or experience. The second part, that is harder to do and less well known, and that is instead of thinking in a way that breaks dowN. There is a scientific model that looks at race separately from gender etc. Rather than trying to figure out which part is which, the goal is to treat the whole person. Modeling intersectionality has become difficult because of the subjectivity of the groups. The need to pay better attention to the inequities among women that are caused by racism, colonialism, ethnocentrism, heterosexism, and able-bodism, is confronting feminist health researchers and activists head on (Havkinsky). In order for intersectionality to be fully acknowledged more effective methodology must be developed. More work is also required to develop effective ways to use quantitative, qualitative, and/or mixed methods to transcend singular categories of social identity such as gender, so that the consequences of the complex combination of various oppressions is captured. Therefore, power, privilege, and intersecting domains of inclusion, exclusion, and health inequalities are better comprehended and addressed.
The problem with mental illness is that it is not talked about enough,especially within ethnic and racial minority groups. Cultural stigma often debases mental illness and considers it to be a weakness or human flaw. This leads to those suffering, feeling ashamed and in fear of reaching out for help. Something must be done to combat this stigma. Intersectionality has become a vital aspect of society as it grows. Mental health inequalities are strongly associated and embedded within the broader social and economic context. It is important to acknowledge each part of a person’s identity to make them comfortable and assure that they are understood. Current treatment of mental illness ignores the effects of social identities on one’s condition. In order to develop more successful methodologies of diagnosis and treatment of mental illness, researchers must explore intersectionality. Mental illness cannot be eradicated from the world, but it can be made better for those living with it.
Similar Articles
JOIN THE DISCUSSION
This article has 0 comments.
